Recommended Global Neuroscience Webinars & Conferences
Asia Pacific & Middle East
NEUROLOGY-2026
- Welcome Message
- About Neurology-2026
- Why Attend Neurology-2026?
- Sessions & Tracks
- AI Sessions
- Market Analysis Report
- Past Conference Report
Welcome Message
On behalf of the organizing committee, we are delighted to welcome you to the 38th World Conference on Neurology, taking place on June 22-23, 2026, in the vibrant city of Barcelona, Spain.
This year, our conference theme is: “Neurology in the Age of AI: Advancing from Insight to Innovation.”
As we stand at the intersection of neuroscience and artificial intelligence, this conference aims to bring together leading neurologists, researchers, clinicians, and innovators from around the world. Together, we will explore cutting-edge research, share groundbreaking discoveries, and discuss transformative approaches that are shaping the future of neurological science and patient care.
We look forward to inspiring sessions, thought-provoking discussions, and meaningful collaborations that will propel the field of neurology forward. Your participation and contributions are key to making this event a remarkable platform for knowledge exchange and innovation.
Welcome to Barcelona, and welcome to the 38th World Conference on Neurology—where insight meets innovation.
About Neurology-2026
Neurology-2026, the 38th World Conference on Neurology, is scheduled for June 22-23, 2026, in Barcelona, Spain. This global gathering serves as a leading platform for neurologists, neuroscientists, clinicians, researchers, and healthcare professionals to exchange knowledge, explore innovations, and advance the frontiers of neurological science.
With the theme “Neurology in the Age of AI: Advancing from Insight to Innovation,” the conference will focus on the intersection of neuroscience and artificial intelligence, highlighting breakthroughs in research, diagnosis, treatment, and patient care.
Neurology-2026 will feature:
- Keynote lectures by world-renowned experts
- Interactive workshops on emerging neurological techniques
- Panel discussions on cutting-edge research and clinical practice
- Poster presentations showcasing innovative studies
This conference provides a unique opportunity to network with global leaders, foster collaborations, and gain insights into the latest developments that are shaping the future of neurology.
Why Attend Neurology-2026?
- Learn from world-renowned neurologists and AI specialists.
- Explore cutting-edge innovations in neurology and AI applications.
- Network globally with researchers, clinicians, and industry leaders.
- Participate in interactive workshops, panels, and poster sessions.
- Showcase your research to a global audience.
- Gain practical insights to enhance clinical practice and research.
- Experience the culture and vibrancy of Barcelona.
What Makes Neurology-2026 Special:
- Theme-focused: “Neurology in the Age of AI: Advancing from Insight to Innovation.”
- Global collaboration with participants from all over the world.
- Comprehensive coverage of all key areas in neurology.
- Platform for inspiration and innovation in research and patient care.
- Neurology Residents and Fellows
- Patients and Caregivers
- Pharmaceutical and Biotechnology Professionals
- Nurses and Nurse Practitioners
- Rehabilitation Engineers
- Radiologists and Imaging Technologists / Specialists
- Genetic Counselors
- Industry Representatives
- Neuromuscular Specialists
- Rehabilitation Specialists
- Neuroscientists
- Neurology-related Allied Health Professionals
- Neurologists
- Neurosurgeons
- Neuropsychologists
- Neurophysiologists
- Physical Therapists and Occupational Therapists
- Speech-Language Pathologists
- AI Specialists
- Psychiatrists
- Psychologists
- Healthcare Professionals
- Medical Students
Sessions & Tracks
Track 01. Neurodegenerative Disorders
Neurodegenerative disorders are a diverse group of progressive conditions characterized by the gradual loss of structure or function of neurons, including cell death. These disorders include Alzheimer’s disease, Parkinson’s disease, Huntington’s disease, amyotrophic lateral sclerosis (ALS), and frontotemporal dementia. They primarily affect older adults but can also present in younger populations depending on genetic or environmental factors. The pathophysiology often involves protein misfolding, mitochondrial dysfunction, oxidative stress, and neuroinflammation, leading to neuronal degeneration in specific brain regions. Symptoms vary depending on the disorder but commonly include cognitive decline, memory impairment, motor dysfunction, behavioral changes, and autonomic disturbances. Diagnosis typically combines clinical evaluation with advanced neuroimaging, genetic testing, and biomarkers. Research in neurodegenerative disorders is rapidly advancing, with an emphasis on understanding disease mechanisms to develop disease-modifying therapies. Emerging therapies include immunotherapy targeting misfolded proteins, gene therapy, neuroprotective agents, and precision medicine approaches. Early detection is crucial to improving outcomes and slowing disease progression. Patient management often requires a multidisciplinary approach, including neurologists, psychiatrists, physical and occupational therapists, speech-language pathologists, and caregivers, aiming to maintain functional independence and quality of life. In addition, lifestyle interventions such as cognitive stimulation, physical activity, and nutrition have shown potential in mitigating disease progression. Neurodegenerative disorders represent a major public health challenge due to their increasing prevalence and socio-economic impact. Research, clinical trials, and advances in diagnostic technologies are essential to combating these complex diseases, providing hope for improved therapies and patient outcomes in the coming years.
Track 02. Stroke & Cerebrovascular Disorders
Stroke and cerebrovascular disorders encompass conditions caused by impaired blood flow to the brain, leading to tissue damage and neurological deficits. Stroke is the second leading cause of death globally and a major contributor to long-term disability. There are two main types: ischemic stroke, resulting from arterial blockage, and hemorrhagic stroke, caused by blood vessel rupture. Risk factors include hypertension, diabetes, hyperlipidemia, smoking, atrial fibrillation, and genetic predispositions. Clinically, patients may present with sudden weakness, numbness, speech difficulties, vision problems, or loss of coordination, depending on the brain region affected. Rapid diagnosis and intervention are critical; ischemic strokes may benefit from thrombolysis or mechanical thrombectomy, while hemorrhagic strokes often require surgical intervention and meticulous blood pressure management. Advanced imaging techniques such as CT, MRI, and perfusion studies play a pivotal role in diagnosis, guiding treatment decisions. Post-stroke rehabilitation is crucial for functional recovery, incorporating physical, occupational, and speech therapies, alongside cognitive and psychological support. Prevention strategies, including lifestyle modifications, pharmacotherapy for hypertension and anticoagulation for atrial fibrillation, are essential to reduce recurrence. Recent advances include AI-assisted imaging for faster detection, tele-stroke networks for timely intervention, and novel therapeutics aimed at neuroprotection and neural repair. Stroke research increasingly focuses on understanding the mechanisms of neuronal injury, neuroplasticity, and recovery, offering hope for more effective therapies and improved long-term outcomes. Multidisciplinary care, patient education, and early rehabilitation remain central to optimizing recovery and quality of life for stroke survivors.
Track 03. Epilepsy & Seizure Disorders
Epilepsy is a neurological disorder characterized by recurrent, unprovoked seizures resulting from abnormal electrical activity in the brain. Seizures can vary widely in type and severity, from brief lapses of attention or muscle jerks to prolonged convulsions, depending on the affected brain region. Epilepsy may result from genetic mutations, structural brain abnormalities, infections, metabolic disorders, or traumatic brain injury. Diagnosis relies on clinical history, neurological examination, electroencephalography (EEG), and neuroimaging to identify structural causes or epileptogenic zones. Management includes anti-epileptic medications, lifestyle modifications, and, in refractory cases, surgical interventions such as resective surgery, vagus nerve stimulation, or responsive neurostimulation. Recent advances in precision medicine and genetics allow for targeted therapies tailored to specific epilepsy syndromes. Pediatric epilepsy presents unique challenges, including developmental and cognitive impacts, necessitating multidisciplinary care involving neurologists, neuropsychologists, and therapists. Quality of life, seizure control, and safety remain central goals, with patient and caregiver education being vital. Emerging research focuses on novel drug targets, neuromodulation, seizure prediction using AI algorithms, and the role of neuroinflammation in epilepsy pathophysiology. Public awareness, early diagnosis, and access to care are critical in reducing morbidity and stigma associated with epilepsy. With ongoing advances in neurotechnology, pharmacotherapy, and personalized care approaches, the management of epilepsy and seizure disorders continues to evolve, offering improved outcomes and hope for patients worldwide.
Track 04. Neuroimmunology & Multiple Sclerosis
Neuroimmunology is the study of interactions between the nervous system and the immune system, encompassing a broad range of autoimmune and inflammatory neurological disorders. Multiple Sclerosis (MS) is the most common neuroimmunological disorder, characterized by demyelination and axonal damage in the central nervous system. The disease often presents in young adults and can lead to physical disability, cognitive impairment, and fatigue. The pathogenesis involves immune-mediated attacks on myelin and oligodendrocytes, influenced by genetic susceptibility and environmental triggers such as viral infections and vitamin D deficiency. Diagnosis relies on clinical assessment, MRI imaging to detect lesions, cerebrospinal fluid analysis, and evoked potentials. Management includes disease-modifying therapies (DMTs) that reduce relapse rates and slow progression, corticosteroids for acute exacerbations, and symptomatic treatments for spasticity, pain, and fatigue. Neuroimmunology also encompasses conditions such as neuromyelitis optica spectrum disorder (NMOSD), autoimmune encephalitis, and peripheral neuropathies. Emerging therapies target specific immune pathways, including monoclonal antibodies and small molecules that modulate immune responses. Advances in biomarker research, MRI techniques, and immunogenetics improve early diagnosis, disease monitoring, and personalized treatment. Multidisciplinary care, including neurology, rehabilitation, psychiatry, and occupational therapy, is essential to optimize functional outcomes. Research continues to explore the mechanisms of neuroinflammation, remyelination, and neuroprotection, offering hope for novel therapies and improved quality of life for patients with MS and other neuroimmunological disorders.
Track 05. Pediatric Neurology
Pediatric neurology focuses on the diagnosis and management of neurological disorders in infants, children, and adolescents. This subspecialty addresses a wide spectrum of conditions, including epilepsy, cerebral palsy, neurogenetic disorders, developmental delays, neuromuscular diseases, and metabolic or autoimmune disorders affecting the nervous system. Children often present with atypical symptoms, and early recognition is crucial to prevent long-term disability and optimize development. Diagnosis involves detailed clinical assessment, neuroimaging, electrophysiology, metabolic and genetic testing, and developmental evaluations. Management strategies are multidisciplinary, combining pharmacotherapy, surgical interventions, physical and occupational therapy, speech therapy, and neurobehavioral support. Pediatric neurologists collaborate closely with families, educators, and allied health professionals to provide individualized care plans that address both medical and developmental needs. Emerging areas include gene therapy for inherited disorders, precision medicine for epilepsy syndromes, and neurorehabilitation technologies such as robotics and virtual reality to enhance motor and cognitive outcomes. Pediatric neurology also emphasizes early intervention programs, seizure control, and preventive strategies for neurodevelopmental disorders. Research focuses on understanding brain development, the impact of genetic and environmental factors, and innovative therapies to improve functional outcomes. With advances in neuroimaging, genomics, and neurotechnology, pediatric neurology continues to evolve, offering hope for improved diagnosis, treatment, and quality of life for children affected by neurological disorders.
Track 06. Neuro-oncology
Neuro-oncology is the study and treatment of tumors of the central and peripheral nervous system, including brain and spinal cord neoplasms. These tumors may be primary, originating from neural tissue, or secondary, representing metastases from systemic cancers. Common primary tumors include glioblastomas, astrocytomas, meningiomas, and medulloblastomas, each with distinct biological behavior, prognosis, and treatment strategies. Neuro-oncology integrates neurosurgery, radiation therapy, chemotherapy, and increasingly, targeted molecular therapies and immunotherapies to optimize patient outcomes. Diagnosis involves neuroimaging, particularly MRI and PET scans, alongside biopsy and histopathological analysis. Molecular profiling and genetic testing help guide precision medicine approaches, enabling personalized therapy. Clinical presentation varies depending on tumor location and size, with symptoms ranging from headaches, seizures, and cognitive deficits to motor and sensory impairments. Multidisciplinary care is essential, involving neurosurgeons, neurologists, oncologists, radiologists, pathologists, and rehabilitation specialists. Recent advances include minimally invasive surgical techniques, stereotactic radiosurgery, immune checkpoint inhibitors, CAR-T cell therapy, and AI-assisted imaging for tumor detection and monitoring. Neuro-oncology research focuses on understanding tumor biology, resistance mechanisms, and developing innovative therapies to improve survival and quality of life. Palliative care and supportive interventions are also critical, addressing pain management, neurological deficits, and emotional well-being. Neuro-oncology represents a rapidly evolving field where translational research, technological innovation, and patient-centered care converge to advance therapeutic outcomes.
Track 07. Neurocritical Care & Emergency Neurology
Neurocritical care and emergency neurology focus on the acute management of life-threatening neurological conditions requiring immediate intervention. This field encompasses stroke, traumatic brain injury, subarachnoid hemorrhage, status epilepticus, acute encephalopathy, and other neurological emergencies. Rapid diagnosis and timely intervention are critical to minimize neuronal damage and improve functional outcomes. Care involves specialized neurointensive care units equipped with continuous monitoring of intracranial pressure, cerebral perfusion, and vital parameters. Multidisciplinary teams including neurologists, neurosurgeons, critical care specialists, nurses, and rehabilitation therapists work together to provide comprehensive care. Neuroimaging, including CT, MRI, and angiography, plays a pivotal role in diagnosis and treatment planning, while laboratory and electrophysiological studies support rapid decision-making. Treatment strategies may include thrombolysis, endovascular interventions, surgical decompression, seizure management, and targeted neuroprotective therapies. Emerging technologies such as AI-assisted imaging, tele-neurology for remote consultation, and predictive analytics enhance diagnostic speed and clinical decision-making. Post-acute rehabilitation and long-term follow-up are essential for functional recovery and quality of life. Research in neurocritical care focuses on optimizing early intervention, understanding secondary brain injury mechanisms, and developing innovative monitoring and therapeutic strategies. Neurocritical care is vital for reducing morbidity and mortality in acute neurological conditions, bridging emergency medicine and specialized neurology for improved patient outcomes.
Track 08. Neuroimaging & Diagnostics
Neuroimaging and diagnostics play a central role in modern neurology, enabling visualization and evaluation of brain and spinal cord structure, function, and pathology. Techniques include magnetic resonance imaging (MRI), functional MRI (fMRI), computed tomography (CT), positron emission tomography (PET), diffusion tensor imaging (DTI), and advanced electrophysiological methods such as EEG and EMG. Neuroimaging assists in diagnosing stroke, tumors, neurodegenerative diseases, epilepsy, and traumatic injuries, guiding clinical management and surgical planning. Functional imaging, including fMRI and PET, allows mapping of brain activity, connectivity, and metabolic processes, supporting research and personalized medicine approaches. Advanced imaging biomarkers facilitate early detection of neurodegenerative diseases, treatment monitoring, and prognostication. Neurodiagnostic tools such as EEG and EMG assess electrical activity and neuromuscular function, aiding in the evaluation of seizures, neuropathies, and movement disorders. Integration of artificial intelligence and machine learning into neuroimaging enhances pattern recognition, predictive analytics, and diagnostic accuracy. Emerging modalities such as optical coherence tomography (OCT) and molecular imaging further expand the scope of neurological assessment. Neuroimaging is critical not only for diagnosis but also for understanding disease mechanisms, evaluating therapeutic interventions, and supporting translational research. Continuous technological innovation and AI integration are transforming neurodiagnostics, providing clinicians with faster, more precise, and personalized insights into neurological disorders.
Track 09. Neurogenetics & Genomics
Neurogenetics and genomics focus on understanding the genetic basis of neurological disorders and applying this knowledge to diagnosis, treatment, and prevention. Many neurological conditions, including epilepsy, neurodegenerative diseases, neuromuscular disorders, and developmental brain disorders, have a genetic component. Advances in next-generation sequencing, whole-exome and whole-genome sequencing, and gene expression profiling have revolutionized the identification of disease-causing mutations and risk variants. Neurogenetic testing allows for early diagnosis, family counseling, and personalized treatment strategies. Gene therapy, RNA-based interventions, and CRISPR technology are emerging as potential curative approaches for monogenic neurological disorders. Neurogenomics research explores the interplay between genes, epigenetics, and environmental factors in the development and progression of neurological diseases. Ethical considerations, including genetic privacy, informed consent, and implications for family members, are central to clinical practice. Collaboration between neurologists, geneticists, molecular biologists, and bioinformaticians is essential for translating genetic discoveries into clinical care. Neurogenetics also plays a vital role in understanding disease mechanisms, identifying biomarkers, and developing targeted therapies. Pediatric populations particularly benefit from early genetic evaluation, enabling interventions that improve developmental outcomes. As genomic technologies advance, neurogenetics promises to enhance precision medicine in neurology, offering hope for improved diagnosis, individualized treatment, and prevention of inherited neurological disorders.
Track 10. Movement Disorders & Neuromodulation
Movement disorders encompass a wide range of neurological conditions characterized by abnormal voluntary or involuntary movements, including Parkinson’s disease, dystonia, tremor, Huntington’s disease, and chorea. These disorders arise from dysfunction in basal ganglia circuits, cerebellum, or related motor pathways. Clinical manifestations vary from rigidity, bradykinesia, and tremor to involuntary movements affecting daily functioning. Diagnosis involves careful clinical evaluation, neuroimaging, electrophysiology, and genetic testing where appropriate. Management strategies are multidisciplinary and may include pharmacotherapy, physical therapy, occupational therapy, and lifestyle interventions. Neuromodulation techniques, such as deep brain stimulation (DBS), transcranial magnetic stimulation (TMS), and vagus nerve stimulation, are increasingly used to modulate dysfunctional neural circuits and improve motor symptoms. Recent advances in wearable sensors and AI-assisted movement analysis support real-time monitoring and personalized therapy adjustments. Rehabilitation strategies focus on maintaining mobility, coordination, and functional independence, while addressing non-motor symptoms such as depression, cognitive impairment, and sleep disturbances. Research continues to explore the pathophysiology of movement disorders, optimize neuromodulation techniques, and develop disease-modifying therapies. Movement disorders and neuromodulation represent a dynamic area in neurology where clinical care, technological innovation, and research converge to enhance patient outcomes and quality of life.
Track 11. Neurorehabilitation & Therapy
Neurorehabilitation focuses on the restoration, compensation, and optimization of function in patients with neurological disorders or injuries, aiming to improve independence, quality of life, and participation in daily activities. This field addresses a wide range of conditions, including stroke, traumatic brain injury, spinal cord injury, cerebral palsy, multiple sclerosis, and neurodegenerative diseases. Neurorehabilitation is inherently multidisciplinary, involving neurologists, physiatrists, physical and occupational therapists, speech-language pathologists, psychologists, and social workers. Treatment strategies include physical therapy to improve strength, coordination, and mobility; occupational therapy to enhance daily living skills; and speech-language therapy to address communication and swallowing difficulties. Cognitive rehabilitation targets memory, attention, and executive function deficits. Innovative approaches such as robotic-assisted therapy, virtual reality, brain-computer interfaces, and telerehabilitation are increasingly being used to augment traditional methods, providing personalized and adaptive therapy. Pharmacological interventions may also support functional recovery by reducing spasticity, managing pain, or enhancing neuroplasticity. Early and intensive rehabilitation is critical, as neuroplasticity—the brain’s ability to reorganize neural networks—is greatest shortly after injury. Outcome measurement relies on standardized functional scales, patient-reported outcomes, and objective performance metrics. Research in neurorehabilitation continues to explore optimal therapy intensity, timing, and integration of technological adjuncts to maximize recovery. With a patient-centered, evidence-based approach, neurorehabilitation empowers individuals to regain functional abilities, participate actively in society, and achieve the highest possible quality of life after neurological injury or illness.
Track 12. Neuroinformatics & AI in Neurology
Neuroinformatics and AI in neurology represent the convergence of neuroscience, data science, and computational technology, aimed at enhancing understanding, diagnosis, and treatment of neurological disorders. Neuroinformatics involves the collection, integration, and analysis of large-scale neurological data, including neuroimaging, electrophysiological recordings, genomics, and clinical records. Artificial intelligence, including machine learning and deep learning, is increasingly applied to identify patterns, predict disease progression, and personalize treatment plans. Applications include automated analysis of MRI and CT scans, seizure prediction in epilepsy, early detection of neurodegenerative diseases, and optimization of rehabilitation strategies. AI-driven neuroinformatics platforms enable integration of heterogeneous datasets, facilitating translational research and supporting clinical decision-making. Ethical and regulatory considerations, including patient data privacy, algorithm transparency, and clinical validation, are critical for safe implementation. Emerging areas include brain-computer interfaces, virtual simulations for neurological training, and predictive analytics for population health management. Collaboration between neurologists, data scientists, engineers, and bioinformaticians is essential to translate computational insights into practical clinical tools. By leveraging AI and neuroinformatics, neurology is moving toward precision medicine, with improved diagnostic accuracy, treatment personalization, and accelerated research. These technologies are also enabling remote monitoring, tele-neurology, and enhanced access to neurological care globally, transforming patient management and advancing the frontiers of neuroscience.
Track 13. Neuropsychiatry & Mental Health
Neuropsychiatry explores the interface between neurology and psychiatry, focusing on the assessment and management of psychiatric symptoms arising from neurological disorders. Conditions in this domain include mood disorders, anxiety, psychosis, cognitive dysfunction, and behavioral changes resulting from neurodegenerative diseases, stroke, traumatic brain injury, epilepsy, and multiple sclerosis. Neuropsychiatrists evaluate how structural and functional changes in the nervous system contribute to psychiatric presentations, employing clinical assessment, neuroimaging, neuropsychological testing, and electrophysiological studies. Treatment strategies are multidisciplinary, integrating pharmacotherapy, psychotherapy, cognitive rehabilitation, neuromodulation techniques such as transcranial magnetic stimulation (TMS), and lifestyle interventions. Attention to psychosocial factors, caregiver support, and quality of life is central. Neuropsychiatry also investigates neurobiological mechanisms underlying psychiatric symptoms, including neurotransmitter dysregulation, neuroinflammation, and network connectivity alterations. Research emphasizes early detection of cognitive and psychiatric complications in neurological diseases, as well as developing targeted therapies and personalized interventions. Emerging trends include digital mental health tools, AI-assisted diagnosis, and biomarkers for predicting disease progression. Neuropsychiatry bridges the gap between brain and behavior, offering a holistic approach to patient care, improving functional outcomes, and addressing the mental health needs of individuals with neurological disorders.
Track 14. Functional Neurological Disorders
Functional neurological disorders (FND) are conditions in which patients experience neurological symptoms, such as weakness, movement abnormalities, sensory disturbances, or non-epileptic seizures, without evidence of structural brain pathology. FND represents a complex interplay of neurological, psychological, and environmental factors, often presenting diagnostic challenges due to symptom variability and overlap with organic conditions. Diagnosis is primarily clinical, based on positive signs such as inconsistency, incongruence with known neurological patterns, and distinctive examination findings. Neuroimaging and electrophysiological studies are typically normal, helping to exclude structural disease. Management is multidisciplinary, involving neurologists, psychiatrists, psychologists, physical therapists, and occupational therapists. Evidence-based approaches include cognitive-behavioral therapy, physiotherapy focused on retraining normal movement patterns, and psychoeducation for patients and caregivers. Early recognition and intervention are associated with better outcomes. Research is increasingly exploring the neural mechanisms underlying FND, including abnormal brain connectivity, altered attention, and impaired motor control networks. Public and professional awareness remains critical to reduce stigma and improve access to care. Functional neurological disorders exemplify the importance of integrating neurological and psychological perspectives, emphasizing patient-centered care, multidisciplinary collaboration, and ongoing research to understand mechanisms and optimize treatment.
Track 15. Rare & Orphan Neurological Disorders
Rare and orphan neurological disorders are conditions that affect a small proportion of the population but often have profound impacts on patients and families. These include rare genetic syndromes, metabolic disorders, neuromuscular diseases, leukodystrophies, and uncommon forms of epilepsy, ataxia, or movement disorders. Despite their low prevalence, these disorders often present diagnostic challenges due to phenotypic heterogeneity, limited clinical awareness, and lack of standardized treatment guidelines. Early and accurate diagnosis is critical and increasingly relies on advanced genetic testing, molecular diagnostics, neuroimaging, and biomarkers. Management is multidisciplinary, combining symptomatic therapy, disease-modifying treatments where available, rehabilitation, and psychosocial support. Research and clinical trials play a pivotal role, often leveraging international collaboration to overcome challenges posed by small patient populations. Patient registries, rare disease networks, and AI-assisted data analysis are transforming understanding and treatment development. Orphan drug development incentives have also accelerated the creation of targeted therapies for these conditions. Clinicians must adopt individualized care approaches, focusing on functional outcomes, quality of life, and family support. Education, advocacy, and public awareness are essential to improve access to care and resources. Rare and orphan neurological disorders exemplify the complexity and diversity of neurology, highlighting the need for innovation, collaboration, and patient-centered approaches to advance diagnosis, treatment, and research.
Track 16. Traumatic Brain Injury & Concussion
Traumatic brain injury (TBI) and concussion represent a major public health concern worldwide, resulting from external mechanical forces impacting the brain. These injuries range from mild concussions to severe brain damage, leading to cognitive, motor, sensory, and emotional impairments. The pathophysiology of TBI involves primary injury from mechanical forces and secondary injury caused by neuroinflammation, oxidative stress, excitotoxicity, and blood-brain barrier disruption. Concussions, a mild form of TBI, are often underdiagnosed yet can have significant short- and long-term consequences, including post-concussion syndrome and increased susceptibility to neurodegenerative diseases. Diagnosis relies on clinical evaluation, neuroimaging, and neurocognitive assessment, often supplemented by biomarkers for neuronal injury. Management is multidisciplinary, focusing on acute stabilization, symptom management, cognitive rehabilitation, physical therapy, and psychological support. Emerging technologies, such as wearable sensors, AI-driven predictive models, and virtual reality-based rehabilitation, improve assessment, monitoring, and functional recovery. Research emphasizes understanding injury mechanisms, identifying biomarkers, optimizing early intervention, and preventing long-term sequelae. Education on injury prevention, return-to-play protocols in sports, and workplace safety measures is critical. The ultimate goal is to minimize functional impairment, enhance neuroplasticity, and promote optimal recovery, making TBI and concussion care a dynamic intersection of neurology, rehabilitation, and technology.
Track 17. Peripheral Neuropathy & Neuromuscular Disorders
Peripheral neuropathy and neuromuscular disorders encompass a broad spectrum of conditions affecting the peripheral nerves, neuromuscular junctions, and skeletal muscles. Peripheral neuropathies may arise from diabetes, infections, autoimmune diseases, toxins, or hereditary conditions, causing sensory disturbances, weakness, pain, and autonomic dysfunction. Neuromuscular disorders include myasthenia gravis, muscular dystrophies, amyotrophic lateral sclerosis, and congenital myopathies. Diagnosis involves clinical examination, electrophysiological testing (EMG, nerve conduction studies), genetic testing, muscle biopsy, and imaging when indicated. Management is tailored to the underlying etiology and often includes pharmacotherapy, immunotherapy, physical therapy, occupational therapy, and supportive interventions. Advances in genetic testing and molecular diagnostics have improved identification of inherited neuromuscular disorders, enabling targeted therapies and early intervention. Emerging treatments include gene therapy, enzyme replacement, and stem cell approaches, offering hope for disease modification and functional improvement. Rehabilitation focuses on preserving strength, mobility, and quality of life. Multidisciplinary care, including neurologists, physiatrists, therapists, and nutritionists, is essential for optimal outcomes. Research continues to explore pathophysiological mechanisms, novel therapeutic strategies, and biomarkers for early detection and monitoring. Peripheral neuropathy and neuromuscular disorders highlight the complexity of the neuromuscular system and the need for integrated clinical care, technological innovation, and patient-centered approaches to enhance function, independence, and well-being.
Track 18. Sleep Disorders & Circadian Neurology
Sleep disorders and circadian neurology focus on the study and management of conditions affecting sleep quality, duration, and timing, which are critical for neurological health. Common disorders include insomnia, sleep apnea, narcolepsy, restless legs syndrome, parasomnias, and circadian rhythm disorders. Sleep disturbances are closely linked to neurodegenerative diseases, stroke, epilepsy, and psychiatric conditions, highlighting the bidirectional relationship between sleep and neurological function. Diagnosis involves detailed sleep history, polysomnography, actigraphy, and assessment of circadian patterns. Treatment strategies are multidisciplinary, encompassing behavioral interventions, cognitive-behavioral therapy for insomnia, pharmacotherapy, positive airway pressure therapy for sleep apnea, and chronotherapy to realign circadian rhythms. Emerging approaches include wearable sleep-tracking technology, AI-assisted sleep analysis, and personalized interventions targeting genetic or metabolic contributors. Understanding the neurobiology of sleep—particularly the role of the hypothalamus, brainstem, and thalamocortical circuits—guides the development of novel therapies. Sleep medicine in neurology also emphasizes prevention, early identification, and management of comorbidities, recognizing the profound impact of sleep on cognitive function, mood, and overall neurological health. Research is exploring the role of sleep in neuroplasticity, memory consolidation, and clearance of neurotoxic proteins such as beta-amyloid, with implications for neurodegenerative disease prevention. Effective sleep management enhances quality of life, cognitive performance, and disease outcomes, positioning sleep neurology as a critical component of comprehensive neurological care.
Track 19. Headache & Migraine Disorders
Headache and migraine disorders are among the most prevalent neurological conditions, affecting millions worldwide and contributing to significant disability and economic burden. Migraines are characterized by recurrent, moderate-to-severe headache attacks, often accompanied by nausea, photophobia, phonophobia, and aura symptoms. Tension-type headaches, cluster headaches, and secondary headaches from underlying pathology also fall under this domain. Pathophysiology involves complex interactions between vascular, neuronal, and inflammatory pathways, including activation of trigeminovascular circuits, cortical spreading depression, and neurotransmitter imbalances. Diagnosis relies on clinical criteria, headache diaries, and exclusion of secondary causes via imaging or laboratory studies. Management is multifaceted, including acute pharmacotherapy (triptans, NSAIDs), preventive treatments (beta-blockers, CGRP inhibitors, anticonvulsants), lifestyle modification, and behavioral therapies. Emerging therapies focus on neuromodulation devices, CGRP-targeted therapies, and precision medicine approaches based on genetic and biomarker profiling. Patient education, lifestyle counseling, and identification of triggers play a critical role in reducing attack frequency and severity. Multidisciplinary approaches integrate neurologists, pain specialists, psychologists, and physical therapists to address both pain and associated disability. Research continues to investigate mechanisms of migraine chronification, novel therapeutics, and the impact of headache disorders on cognitive function and mental health. Advances in imaging, neurophysiology, and molecular biology are providing deeper insights, enhancing diagnosis, prevention, and individualized treatment strategies.
Track 20. Neurovascular Interventions
Neurovascular interventions and endovascular therapies focus on minimally invasive techniques to diagnose and treat cerebrovascular diseases, including ischemic stroke, aneurysms, arteriovenous malformations, and carotid artery disease. Endovascular procedures, such as mechanical thrombectomy, coil embolization, stent-assisted angioplasty, and flow diversion, offer life-saving and function-preserving alternatives to traditional surgery. Advances in imaging, including CT angiography, MR angiography, and digital subtraction angiography, guide precise navigation and intervention. Patient selection, timing, and multidisciplinary collaboration between neurologists, neurosurgeons, interventional radiologists, and critical care specialists are critical to achieving optimal outcomes. These interventions reduce morbidity and mortality in acute stroke and other cerebrovascular emergencies, particularly when performed in specialized neurovascular centers. Emerging technologies include robotic-assisted endovascular devices, AI-guided imaging interpretation, and novel embolic and stent materials to improve safety and efficacy. Post-procedure care emphasizes neurological monitoring, antithrombotic management, and rehabilitation to restore function. Research continues to refine procedural techniques, expand treatment windows, and enhance patient outcomes. Neurovascular interventions exemplify the intersection of advanced technology, clinical expertise, and patient-centered care, providing cutting-edge solutions for complex cerebrovascular disorders.
Track 21. Brain-Computer Interfaces & Neurotechnology
Brain-computer interfaces (BCIs) and neurotechnology represent a revolutionary field in neurology, connecting the brain directly with external devices to restore or augment neural function. BCIs translate neural signals into commands for prosthetic limbs, communication devices, or computer systems, providing life-changing solutions for patients with paralysis, spinal cord injury, stroke, or neurodegenerative diseases. Neurotechnology also encompasses neuromodulation tools, wearable sensors, implantable devices, and advanced neuroimaging platforms to monitor and influence brain activity. These technologies rely on electrophysiology, neuroimaging, and computational algorithms, often integrating artificial intelligence for signal processing and adaptive control. Clinical applications include motor rehabilitation, communication for locked-in patients, seizure control in epilepsy, and cognitive enhancement. Ethical and regulatory considerations, including patient safety, privacy, and long-term effects, are central to implementation. Ongoing research focuses on improving signal fidelity, miniaturization of devices, wireless interfaces, and bidirectional BCIs that provide both input and feedback to the nervous system. Neurotechnology also holds promise in neuroscience research, enabling precise mapping of neural circuits, understanding cognition, and testing novel therapeutic strategies. BCIs and neurotechnologies exemplify the convergence of neuroscience, engineering, and computational science, offering transformative solutions for neurological disability, augmenting human capabilities, and paving the way for next-generation neurotherapeutics.
Track 22. Cognitive Neuroscience & Neuroplasticity
Cognitive neuroscience and neuroplasticity explore the neural mechanisms underlying cognition, learning, memory, attention, language, and executive function, while investigating the brain’s ability to reorganize and adapt. Neuroplasticity is fundamental for recovery after brain injury, stroke, or neurodegenerative disease, enabling the formation of new synaptic connections and functional reorganization. Techniques such as functional MRI, EEG, TMS, and PET imaging allow researchers to study brain networks and plastic changes over time. Understanding cognitive processes and plasticity guides interventions including cognitive rehabilitation, neuromodulation, and targeted pharmacotherapy. Environmental enrichment, physical exercise, and behavioral therapies further enhance neuroplasticity. Cognitive neuroscience also informs the design of brain-computer interfaces, neurorehabilitation programs, and AI-assisted cognitive training. Research focuses on age-related cognitive decline, recovery mechanisms after injury, and strategies to promote learning and memory consolidation. Translational applications are central to improving patient outcomes in dementia, stroke, traumatic brain injury, and psychiatric disorders. By bridging basic neuroscience with clinical practice, cognitive neuroscience and neuroplasticity provide insights into brain adaptability, offering innovative therapeutic avenues for restoring function and optimizing mental performance.
Track 23. Neuropharmacology & Drug Development
Neuropharmacology and drug development focus on the study of drugs that influence the nervous system and the creation of new therapeutics for neurological disorders. This field encompasses understanding molecular targets, neurotransmitter systems, receptor signaling, and mechanisms of action for existing and novel drugs. Neuropharmacology addresses a wide range of conditions including epilepsy, Parkinson’s disease, Alzheimer’s disease, multiple sclerosis, neuropathic pain, psychiatric comorbidities, and sleep disorders. Drug development involves preclinical studies, pharmacokinetics, pharmacodynamics, and clinical trials to evaluate efficacy, safety, and tolerability. Advances in molecular biology, genomics, and computational modeling facilitate precision medicine approaches, enabling the design of targeted therapies. Emerging areas include biologics, monoclonal antibodies, gene therapy, and small-molecule modulators. Neuropharmacology also studies drug-drug interactions, side effect management, and long-term safety in chronic neurological conditions. Translational research bridges laboratory discoveries with clinical application, improving treatment outcomes and patient quality of life. Collaboration between neurologists, pharmacologists, molecular scientists, and regulatory experts ensures the development of safe, effective, and innovative therapies. Neuropharmacology is pivotal in advancing neurological care, offering hope for disease-modifying treatments and personalized interventions for complex neurological disorders.
Track 24. Neuroethics & Clinical Guidelines
Neuroethics and clinical guidelines focus on the ethical, legal, and societal aspects of neurological practice, research, and innovation. Neuroethics addresses dilemmas arising from emerging technologies such as brain-computer interfaces, neuroimaging, neuromodulation, genetic testing, AI-assisted diagnostics, and novel therapeutics. Key considerations include patient autonomy, informed consent, privacy, cognitive enhancement, allocation of scarce resources, and the societal impact of neurological interventions. Clinical guidelines provide evidence-based recommendations for the diagnosis, treatment, and management of neurological disorders, ensuring standardized and high-quality care. They integrate current research, expert consensus, and patient-centered perspectives to guide clinical decision-making, optimize outcomes, and reduce variability in care. Neuroethics also explores the implications of predictive diagnostics, gene editing, and neuroenhancement on identity, responsibility, and equity. Ongoing research in this domain informs policy development, public education, and professional training. By combining ethical principles with practical guidelines, neuroethics and clinical frameworks promote responsible innovation, equitable access to care, and patient-centered practice in neurology. These disciplines are critical for navigating the complex interplay of neuroscience, technology, and society while maintaining trust, safety, and professional integrity.
Track 25. Tele-neurology & Digital Health Solutions
Tele-neurology and digital health solutions are transforming the delivery of neurological care, enabling remote assessment, diagnosis, treatment, and monitoring of patients using telecommunication technology. Tele-neurology is particularly valuable for stroke management, chronic neurological conditions, epilepsy, movement disorders, and follow-up care, especially in underserved or remote regions. Digital health tools include teleconsultations, mobile apps for symptom tracking, wearable devices for real-time monitoring, electronic health records integration, and AI-assisted diagnostic platforms. These technologies enhance access to specialized care, reduce healthcare costs, and improve patient engagement and adherence. Tele-neurology allows rapid intervention in acute conditions such as stroke through virtual “telestroke” networks, supporting timely thrombolysis or thrombectomy decisions. Digital platforms facilitate data collection, remote rehabilitation, cognitive training, and patient education. Challenges include maintaining data security, privacy, equitable access, and ensuring clinical accuracy. Research focuses on efficacy, patient satisfaction, cost-effectiveness, and integration with traditional care pathways. Tele-neurology and digital health represent a paradigm shift in neurological care delivery, expanding the reach of specialized services, improving patient outcomes, and fostering innovation in monitoring, diagnostics, and therapy in the modern digital era.
AI Sessions
Submit your abstract for our Neurology 2026 AI sessions and secure your registration for just €499 if accepted. In an era where neurology is increasingly intertwined with AI, don’t miss the chance to connect with the pioneers of tomorrow!
- AI in Neurological Diagnostics
- Machine Learning Applications in Neurology
- AI-Driven Neuroimaging
- AI-Powered Neurotherapies
- Personalized Medicine in Neurology
- AI in Neurodegenerative Disease Management
- Neuroinformatics & Data Analytics
- AI in Neurorehabilitation
- Ethical and Legal Implications of AI in Neurology
- AI and Neuromodulation
- Neural Networks in Neurology
- AI-Augmented Diagnostics
- Future Directions in AI Neurology
- AI in Stroke Management
- Predictive Models in Neurology
- Digital Neurology Platforms
- AI in Pediatric Neurology
- Tele-neurology and AI Integration
- Emerging Trends in AI-Driven Neurology
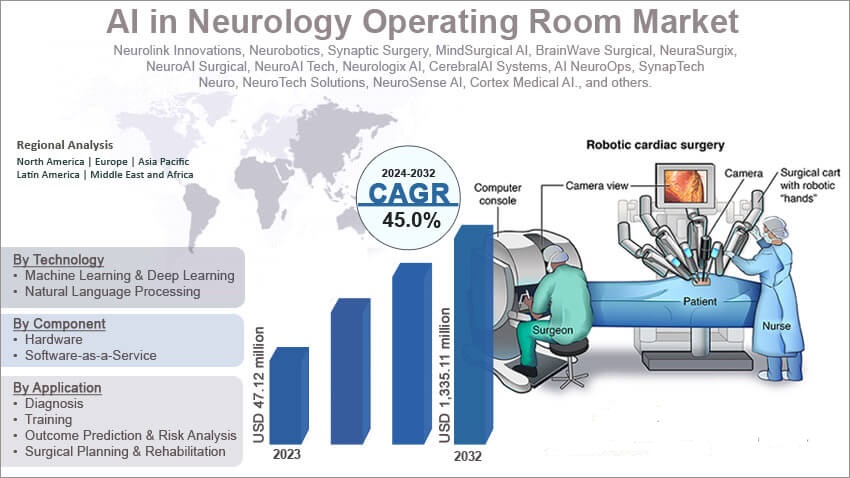
Market Analysis Report
The global neurology market is positioned for strong growth between 2025 and 2030, driven by an aging world population, rising prevalence of neurological disorders such as Alzheimer’s, Parkinson’s, and stroke, and expanding investments in research and clinical care. In 2024, the overall neurology market was valued at approximately USD 63 billion, and it is projected to approach or exceed USD 95 billion by 2029, reflecting an estimated CAGR of about 7.1%. This sustained expansion highlights increasing demand for advanced treatments, diagnostic tools, neuropharmaceuticals, and therapeutic innovations that improve patient outcomes and quality of life.
Within this broader market, neurotechnology stands out as one of the fastest?growing segments. Fueled by breakthroughs in brain?computer interfaces (BCIs), neuromodulation devices, wearable sensors, and digital therapeutics, the neurotechnology sector is anticipated to grow from around USD 15.8 billion in 2025 to over USD 33 billion by 2031, demonstrating a robust CAGR of roughly 13.1%. Parallel to this, the AI in neurology market—encompassing AI?driven diagnostics, predictive analytics, and clinical decision support systems—is forecast to expand at an even higher pace, with a projected CAGR near 28.9%, reaching about USD 2.5 billion by 2030 from a base of approximately USD 0.7 billion in 2025. This trend underscores the rapidly increasing integration of artificial intelligence and machine learning into neurological research and clinical practice.
Other critical sub?segments such as neuroscience tools and platforms and neurodiagnostics are also expected to grow steadily over the next five years. The neuroscience market which includes advanced imaging systems, research instruments, and laboratory technologies is projected to rise from an estimated USD 41.2 billion in 2026 to roughly USD 55.2 billion by 2031, at a CAGR of about 6.0%. The neurodiagnostics sector, focusing on early disease detection technologies and imaging modalities like MRI, CT, EEG, and emerging AI?enhanced systems, is likely to expand from around USD 9.8 billion in 2026 to over USD 13.8 billion by 2031, reflecting ongoing demand for earlier, more accurate, and less invasive diagnostic solutions.
Overall, the neurology landscape over the next five years will be shaped by technological convergence, research breakthroughs, and the increasing adoption of digital health and AI platforms. Growth will be driven not only by clinical needs but also by cross?industry collaboration, including partnerships between healthcare institutions, technology companies, academic research centers, and policymakers. Regions such as North America and Europe are expected to maintain leadership in innovation and market size, while Asia?Pacific markets show rapidly increasing investment and adoption due to expanding healthcare infrastructure and rising patient volumes. Collectively, these trends point to a dynamic and evolving neurology ecosystem that promises both commercial opportunity and significant advancements in patient care.
According to the World Health Organization (WHO), there will be an estimated 55 million dementia patients worldwide in 2022, with 60% of them living in low- and middle-income nations. This figure is projected to increase by 10 million cases every year.
Global & International:
- World Federation of Neurology (WFN)
- Global Neurology Alliance (GNA)
- International Brain Research Organization (IBRO)
- International League Against Epilepsy (ILAE)
- World Stroke Organization (WSO)
- Multiple Sclerosis International Federation (MSIF)
- International Headache Society (IHS)
Regional & Continental:
- American Academy of Neurology (AAN)
- European Academy of Neurology (EAN)
- Asian-Oceanian Association of Neurology (AOAN)
- Pan African Academy of Neurology (PAAN)
- Pan Arab Union of Neurological Societies (PAUNS)
National / Country-Level:
- Indian Academy of Neurology
- Association of British Neurologists
- German Society for Neurology
- Spanish Society of Neurology
- Japanese Society of Neurology
- Chinese Society of Neurology
- Australian & New Zealand Association of Neurologists (ANZAN)
- Brazilian Academy of Neurology
- Egyptian Society of Neurology, Psychiatry & Neurosurgery
- Saudi Neurological Society
- Philippine Neurological Association
- Swedish Neurological Society
Subspecialty / Focused Groups:
- International Neuromodulation Society (INS)
- International Child Neurology Association (ICNA)
- International Parkinson’s and Movement Disorder Society (MDS)
- Functional Neurological Disorder Society (FNDS)
- Peripheral Nerve Society (PNS)
- International Federation of Clinical Neurophysiology (IFCN)
Participants & Participation Options
Speaker
-
Deliver keynote or invited lectures.
-
Share cutting-edge neurological research, innovations, and insights with global delegates.
Delegate
-
Attend scientific sessions, panel discussions, and networking events.
-
Access conference materials and interact with experts across neurology and neuroscience.
Poster Presenter
-
Showcase original neurological research through printed or digital posters.
-
Engage in one-on-one discussions with attendees and experts.
Exhibitor
-
Display neurology-related products, technologies, or services in dedicated exhibition spaces.
-
Network with delegates, potential clients, and collaborators.
Video Presentation
-
Present neurological research findings or innovations via recorded video sessions.
-
Ideal for participants unable to attend in person.
E-Poster Presenter
-
Share neurological research electronically through interactive e-posters.
-
Participate in virtual discussions and Q&A sessions with attendees.
Virtual Registration
-
Attend live-streamed keynote sessions, scientific presentations, and panel discussions online.
-
Access conference recordings, digital materials, and participate in virtual networking.
-
Ideal for international participants or those unable to attend in person.
- Earn CPD/CME points
- Networking opportunities with global experts and peers
- Certificate of participation
- DOI publication opportunities in conference proceedings
- Access to cutting-edge neurological research
- Professional visibility for speakers, presenters, and exhibitors
- Opportunities for global collaboration
Abstract Submission & Registration Timeline
- Abstract Submission Open: Now Open
- Early Bird Registration: January 22, 2026
- Standard Registration: March 22, 2026
- Final Registration Deadline: June, 2026
Abstract Submission Details:
- All abstracts submitted will undergo a peer-review process to ensure scientific quality and relevance.
- Authors will receive an Abstract Acceptance Letter upon approval, confirming inclusion in the conference program.
- Accepted abstracts will be published in the conference proceedings with DOI, providing global visibility and citation opportunities.
For any questions or assistance regarding the 38th World Conference on Neurology, abstract submission, registration, or participation, please contact:
- Email: contact@neurologyconference.com
- Phone: +44 2880 090005
- Website: https://neurology.global-summit.com/
You can register here: Register for Neurology-2026
Submit your abstract here: Submit Your Abstract
You can also reach out via our social media channels for updates and announcements.
Past Conference Report
NEUROLOGY-2025
The 37th World Conference on Neurology will take place on November 24–25, 2025, in the captivating city of Barcelona, Spain. As a premier global gathering in the field of neurology, this prestigious event will unite leading neurologists, researchers, clinicians, and innovators to explore cutting-edge advancements and the transformative role of artificial intelligence in neurological science.
The conference will feature a comprehensive scientific program that addresses both current challenges and future directions in neurology. Attendees can look forward to dynamic keynote lectures from distinguished experts, interactive panel discussions, and hands-on workshops. Core topics will span a wide range of disciplines, including neurodegenerative diseases, neuroimaging, neurogenetics, and AI-powered diagnostics.
The conference will feature a comprehensive and forward-thinking scientific program, addressing both current challenges and emerging opportunities across all areas of neurology. Attendees can look forward to: Dynamic keynote presentations, Interactive panel discussions, Hands-on workshops and live demonstrations , Symposia on translational neuroscience and precision medicine approaches ,Case studies and real-world applications from clinical settings.
Past Reports Gallery
To Collaborate Scientific Professionals around the World
Conference Date June 22-23, 2026
For Sponsors & Exhibitors
Speaker Opportunity
Useful Links
Supported By
All accepted abstracts will be published in respective Conference Series International Journals.
Abstracts will be provided with Digital Object Identifier by